Vaginal Health
is an important part of a woman's overall wellbeingCFReSHC CF-SRH Resource Guide by Patients for Providers and Patients
Key
For Providers
For Patients
For Patients and Providers
Introduction
Vaginal symptoms can negatively impact fertility, intimate relationships (desire for sex and ability to reach orgasm) and self-confidence.
Researchers indicate that women with CF suffer from multiple vaginal issues. For example, 18% of women with CF report that they experience yeast infections due to frequent antibiotic use for pulmonary exacerbations [1]. A 2001 study in Verona, Italy surveyed 94 CF patients who had received antibiotic therapy in the last year, finding that 61% of the women reported vulvo-vaginal disorders [2]. A French study reported in 2015 that CF patients receiving antibiotic therapy had a “higher incidence of vulvovaginal disorders,” which could be due to the antibiotics destroying protective bacteria in the vagina [3].
A 2018 survey by Kazmerski et al of 188 females with CF in the US found that 49% had had at least one yeast infection; 19% reported at least one yeast infection per year.1 Yeast infections in people with CF often result from antibiotics or corticosteroids, which kill good bacteria, allowing yeast to grow. CF-related diabetes is also a factor in developing yeast infections.2 A 2001 study in Verona,……to the end of the 1st paragraph.
Further, women in the US with CF have reported having thick cervical mucus, which is due to abnormal CFTR function [4]. Thick cervical mucus can make routine pelvic exams painful and can impede fertilization by blocking sperm and/or increasing the amount of time it takes to become pregnant [4]. [see (In)Fertility chapter] Women with CF also experience intimacy issues such as “pain during sex….coughing during sex, excessive flatulence, and coughing up blood during or after sex” [1]. Moreover, Chambers et al found higher rates of dyspareunia and coital incontinence in the CF population than in the general population [5]. Other issues include sexually transmitted infections and cervical dysplasia.
Accessing appropriate care for vaginal symptoms is a concern. In the French study, for instance, researchers examined whether adult female participants (n=120) received adequate gynecological management, finding that: “gynaecological care (frequency of follow-up, cervical screening and contraceptive use among sexually active women) in women with CF fails to reach the recommended level” [6].
Simonnet-Bisson et al. note that patients prioritize gynecological care less than CF-care related problems like lung infections, gastrointestinal problems, or endocrine issues.[3] Thus, they have lower rates of sexually-transmitted infection screening than the general population (19% vs 34%), lower rates of contraceptive use (55% vs 74%), and lower rates of cervical cancer screening or pelvic exams (26% vs 57%).[1,2] Mental health issues may also complicate vaginal health and care. With the advent of CFTR modulator therapy, vaginal health issues for women with CF may change; much of our knowledge is developing or is still unknown.
- Do you have a gynecologist that you see regularly who manages your vaginal health, such as screening for sexually transmitted infections?
- Have you noticed any changes to your vaginal health or menstrual cycle since starting modulators?
- Do you ever have issues with yeast infections or other vaginal infections?
- What do you do when you have symptoms of a vaginal yeast infection? Are you worried about vaginal yeast infection due to antibiotic use? If so, we should discuss treatment options as antifungals may not be an option due to modulator use.
- Do you get routine cervical cancer screening and follow up on abnormal results?
- Have you noticed any changes in your vaginal discharge (i.e., its color, consistency, amount, or odor)?
- Do you use any vaginal cleansers or douches? (Please check with your gynecologist first, as any change in pH can worsen vaginal symptoms.)
- Do you eat a balanced diet? (Diet affects our vaginal area and how much fluid is produced.)
To Gynecologist
- Report any vaginal health issues to your PCP or CF Clinic Provider.
- What methods are used to determine the cause of certain vaginal health issues? (abnormal cervical mucus, vaginal discharge, dryness, itchiness, vaginal pain)?
- If I have a lung infection and am on antibiotics, how might I avoid a yeast infection? Are there any prophylactic ways to prevent this issue?
- Which medications do I take that may contribute to changes in the consistency or odor of vaginal discharge? When should I start being concerned?
Patient to CF Providers:
- I’m noticing vaginal changes since starting a modulator. Is this to be expected/a common side effect?
- Which CF medications result in the development of yeast infections or candidiasis?
- Do any of my CF medications interact with the medications I take for vaginal issues?
Patient to OB/GYNs:
- I have painful sex and it seems that I have vaginal dryness and/or vaginal tightness. Is there a way you can help me to address and manage these symptoms?
- What does my cervical mucus look like now? Is it different from my prior visit?
- A request: My cervical surface is fragile, please be careful if you have to scrape off cervical mucus for this pelvic exam.
Terminology
Understanding vaginal health terminology is key to seeking proper diagnosis and treatment.
VAGINITIS: defined as vaginal inflammation that can result in discharge, itching and pain.
Common types of vaginitis are:
- CFTR – Cystic Fibrosis transmembrane conductance regulator; it maintains the salt and water balance in the body, which ensures the mucus produced in the body is thin.4
- Bacterial Vaginosis: see Causes, Symptoms and Treatment chart
- Yeast Infections: see Causes, Symptoms and Treatment chart
- Trichomoniasis: Caused by a parasite commonly transmitted by sexual intercourse.
- Viral Vaginosis: Viruses of the vagina mostly spread through sexual contact.
VAGINISMUS: A condition in which involuntary muscle spasms prevent vaginal penetration.
VAGINAL ATROPHY: A condition in which the lining of the vagina becomes thinner and drier. Vaginal dryness can be caused by a drop in estrogen levels as a result of menopause, childbirth, or ovary removal. Cervical mucus can be affected by vaginal dryness, antibiotics and transplant medication. Further research is underway to understand the impact of CF modulators on cervical mucus.
- Vaginal Flora – the bacteria that live inside the vagina. Bacteria help maintain a healthy vaginal microbiome.
VULVODYNIA: Chronic pain or discomfort around the opening of the vagina.
Researchers are trying to find the causes of vulvodynia [7]. They may include:
| POSSIBLE CAUSES OF VULVODYNIA | |||
| Allergies or irritation to chemicals or other substances | Abnormal response in vulvar cells to an infection or trauma | Genetic factors that make the vulva respond poorly to a chronic inflammation | Hypersensitivity to yeast infections |
| Muscle spasms | Nerve injury or irritation | Hormonal changes | History of sexual abuse |
| Frequent antibiotic abuse | Weakness of the pelvic floor muscles | Irritation from Candida (yeast) which can cause an area around the vulva to be very sensitive | |
VAGINAL CANCER: A disease in which malignant (cancer) cells form in the vagina. Signs and symptoms include pain and abnormal vaginal bleeding. Pap smear tests can detect cancer. The HPV vaccine is an effective prevention.
VULVAR CANCER: A type of cancer that occurs on the outer surface area of the female genitalia. It commonly occurs as a lump or sore on the vulva that often causes itching. HPV vaccination also prevents vulvar cancer.
SEXUALLY TRANSMITTED INFECTIONS (STI): These infections spread through sexual contact, including intercourse, and require testing by a gynecologist or primary care provider. STIs, such as herpes, can negatively impact vaginal health, potential pregnancy, and sexual partners. Self monitoring can help a woman with CF notice and address potential symptoms with their women’s health provider. Symptoms to report include:
What to know about Vaginal Infections
While the symptoms of bacterial vaginosis (BV) and vaginal yeast infections (VYI) seem similar, there is a difference between these two diagnoses. BV is an imbalance of bacteria that is associated with an increased risk of getting HIV, pelvic inflammatory disease and adverse pregnancy outcomes [8]. VYI are more common due to antibiotic use breaking down healthy bacteria within the body. [See chart for causes, symptoms and treatment for VYI and BV]
While CF clinics may prescribe antifungal remedies while a patient is on antibiotics, clinicians may overlook other conditions, such as BV and sexually transmitted infections (STIs), because diagnosis requires pelvic exams and/or specialized testing [9, 10]. Yet the latter testing may be necessary, not least of which because women with CF can have multiple infections at the same time. Baldwin believes that additional research is needed to better understand the incidence of bacterial vaginosis (BV) and vaginal yeast infections (VYI) in the female CF population [9].
There is a dearth of extant scientific literature about STIs in cystic fibrosis (CF). Unfortunately, human papillomavirus (HPV) infection has a very high prevalence rate worldwide, with over 80% of sexually active adults infected at some point in their life, and is a well-known, necessary (but insufficient) cause for cervical cencer [11, 12]. For its part, herpes simplex virus (HSV) is another very common STI; because of the physical and psychological morbidities associated with it, women with CF should take precautions to prevent its acquisition [13]. These common infections likely impact the lives of sexually active members of the CF community. While women with CF might not want to seek additional specialty care, Dr. Baldwin encourages routine gynecological care to ensure proper diagnostic testing.
| CAUSES, SYMPTOMS AND TREATMENT FOR VYI AND BV | ||
| Vaginal Yeast Infections (VYI) | Bacterial Vaginosis (BV) | |
| Causes | Overgrowth of Candida fungus possibly due to: high blood sugar, antibiotics, pregnancy, birth control pills, hormone replacement therapy | Change in the vaginal pH
e.g. Gardnerella vaginalis bacteria |
| Symptoms |
|
|
| Treatments | Prescribed and over the counter (OTC) medications such as miconazole, monistat or fluconazole. | Always requires prescription medications such as metronidazole, tinidazole and clindamycin. |
A CFReSHC snap poll revealed that 22 of 61 respondents use an antifungal (oral or vaginal cream) routinely or as needed to treat their VYI. Twenty-nine respondents preferred an OTC treatment; 10 used other options such as modifying their diet or using homeopathic treatments [14].
Research on Vaginal Health
Cervical mucus changes according to the fluctuating hormones during the menstrual cycle. As one reaches ovulation, cervical mucus becomes slippery and the color of egg whites, but during the luteal phase (when progesterone rises and estrogen drops), cervical mucus becomes dry until menstruation.[5]
The CFTR protein is present in the endocervical epithelium and fallopian tubes, and this can affect cervical mucus, making it sticky and thick, and increase the risk of cervical dysplasia for women with CF.[3,6] Modulators seem to be changing this profile. Still, poor lung function, frequent exacerbations, hydration levels, diet, medications, pregnancy, and one’s CF genotype can also affect cervical mucus quality.[7] Monitoring cervical mucus quality in females with CF is essential because individuals with CF are prone to develop yeast infections, which makes the cervical mucus appear curdy, accompanied by pain, redness, and swelling.[8]
Kazmerski’s survey on sexual and reproductive health among 188 adolescent girls and young adult women with CF found in 2018 that 18% experienced yeast infections and that only 26% had ever undergone a Pap smear or pelvic exam (unlike 57% of women without CF) [1].
Rousset-Jablonski et al. (2018) report that there is a high percentage of females with CF (FwCF) who have abnormal pap smears and cervical dysplasia. This occurs in both transplanted and non-transplanted females.3,4 Despite this heightened risk, the level of cervical screening in females with CF is inadequate, with only 55% of females having reported a previous pap smear.[4, 5]
Females with CF who are transplanted and taking immunosuppression drugs can also have an even greater risk of cervical dysplasia.[4,6] Because of the positive impact modulator therapy has had on longevity, it has only increased the need for regular Pap smears for females with CF. More broadly, modulator therapy has increased the need to address sexual and reproductive health (SRH) care and decision-making. Indeed, the modulator era has driven a need to consider including SRH issues in delivering CF adolescent and adult care. West et al. and CFReSHC patient-partners both point out that most women with CF want to discuss their SRH care in the CF setting, yet only a minority receive or have such discussions.[4]
- Ovarian dysfunction and decreased ovarian reserve have been documented…cervical mucus and uterine fluid pH (see questions below); changes after HEMT.[5]
- Genital Candidiasis and modulator therapy require adjustments in azole therapy.[4]
A CFReSHC Snap poll (n=80) on the topic of vaginal health indicated that 48.1% of respondents experienced vaginal yeast infections. Yet, sexual and fertility issues are rarely talked about during routine CF clinic visits. Since women with CF are now identifying sexual and reproductive concerns as important to them, it is important to address such symptoms and conditions.
Cervical Mucus
Researchers have found that with the use of modulator therapy, there is a decrease in cervical mucus as compared to previous non-use, and that there is an increase in the pH of mucus viscosity as a result of modulator therapy. Whereas before modulators, women with CF were considered sub-fertile, researchers are now finding that they are fertile.4,7-8 (See Infertility chapter in this guide)
Conditions that Affect Vaginal Health in CF
Numerous conditions can impair one’s vaginal health.
- Vaginal infections. Since people with CF are immunosuppressed, fighting and clearing vaginal infections, like vaginal candidiasis (yeast infection) and bacterial vaginosis, can be more difficult.
- Cervical dysplasia. Pap smears of females with CF have shown a high prevalence of abnormal cells in the cervix. Lee et al. found that among females ≥ 25 years of age, the rate of abnormal cytology among non-transplanted females with CF is almost four times that in the general population.9 This may be caused by an inadequate cervical mucus structure in the body.9
- Menstrual cycles. Regular menstrual cycles have been seen to be associated with better lung function, better BMI, and better vaginal health overall.6 Often, weight fluctuations can cause CF patients to have missed periods (aka amenorrhea). Medications taken can also cause changes to the estrogen levels, which affect the blood volume during menstruation, thus leading to less lubrication and elasticity in the vaginal area.10
- Sexually transmitted infections. Deciding who, when, and how often you have sex is a personal decision, but one must be careful to avoid contracting STIs. STIs include, but are not limited to:
I have had serious issues with recurrence of abnormal pap smear results from persistent HPV. I’ve had to have three back to back colposcopies due to the HPV not clearing, which the doctor attributed to weakened immune system and my Cystic Fibrosis.
Patients should be transparent with their CF care team about their current sexual activity because the team can provide pertinent information to stay healthy. Patients are highly recommended to get the HPV (human papillomavirus) vaccine, Gardasil. HPV has been shown to be harder to clear for people with CF due to their weakened immune system. STIs like HPV can also cause cancers of the skin and genital area if a person eventually gets transplanted (or is already).[11] Pap smears can help detect early abnormalities in the cervix and precancerous or cancerous cells in the vaginal area that are most often caused by HPV.[11]
Modulators’ Effect on Vaginal Health
Modulators have helped thin cervical mucus and cleared yeast infections more easily or prevented them from occurring altogether.[3,5] Patients should be aware that some drugs used to treat yeast infections and vaginosis, like antifungal medications, may interact with modulators.[11]
Modulators have also helped reduce high levels of salt in the vaginal transudate. In so doing, they have mitigated the sense of dryness that many females experienced prior to modulators during sexual relations.[3,12]
Since starting a modulator and having better lung function, it has made it possible to actually discuss other issues when it comes to my gynecological issues. In the past, these were thrown to the wayside due to my pulmonary and CF issues being so prevalent and needing immediate attention all the time. I’m so thankful for modulators because other issues that have always been there (pelvic pain, pregnancy issues, vaginal bacteria/infections) can now be addressed with the adequate concern and attention needed in order to fix or alleviate some of the symptoms.
Sometimes I feel embarrassed when having sex because of how dry I am down there. There is a stigma that when you’re ‘turned on’ that it will show by the wetness down there, so I avoid sex sometimes due to this, and it makes me feel inadequate.
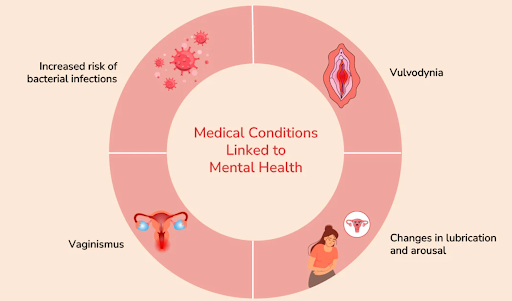
How Does Mental Health Affect Vaginal Health?
Mental health includes one’s emotional, psychological, and social well-being. It affects how a person treats, thinks, and interacts with themselves.[13] Having self-awareness of one’s body can assist with maintaining one’s vaginal health.[14]
Depression and anxiety are common in CF. They stem from various concerns, like deteriorating health, having to worry about being exposed to bacteria that can cause a person to be hospitalized, keeping track of medications, staying on top of treatments, and going to doctor visits.
Experiencing conditions such as vaginal candidiasis, thick cervical mucus, dyspareunia, and vaginal dryness can lead to depression, feeling less satisfied with life, poorer self-esteem, and increased stress levels, which can then interfere with sexual and emotional relationships [1,15].
Depression can affect vaginal health because the brain produces less dopamine and oxytocin in this state.15 Selective Serotonin Reuptake Inhibitors (SSRIs), used to treat depression and anxiety, can cause vaginal dryness, issues with sex drive, and can cause discomfort during penetration.[15] These problems can keep women from seeking additional help or deter them from taking their mental health medications so they can have a more stable vaginal health/sexual drive.
Depression can also impair one’s memory, energy, and executive function and can jeopardize treatment adherence.16 As a result, a person can get a pulmonary exacerbation, which may require antibiotics. A side effect of using antibiotics is fungal vaginitis, which can cause discomfort in the vaginal area and requires treatment.[3]
In their study on intimacy and CF, Simonnet-Bisson et al. found that the primary cause of sexual issues in females with CF is the lack of vaginal lubrication (78.8%). Pain (74.1%) and discomfort are the secondary reasons.[3]
I’ve been hospitalized on numerous occasions for pulmonary exacerbations, and while being treated for my lungs, I developed infections and bacteria (candida) in my vaginal area. This caused persistent itching and I had to be on another antibiotic due to this. This makes me not only uncomfortable but just an inconvenience as one organ (my lungs) got better, another organ had to suffer.
They conducted interviews that revealed that women’s sexual lives were often uncomfortable or painful, unsatisfying, or sex was avoided altogether. Many women either felt sexually different from their peers or betrayed by their bodies.[3]
Aging and Vaginal Health
In October 2016, Healthline writer Annette McDermott described how the vagina is a complex organ that plays a role in sexual pleasure and childbirth. She writes that as you age, your vagina will too [13].
There is a variety of information available about vaginal health and aging, including:
- Estrogen is responsible for keeping the vagina lubricated, elastic, and acidic.
- The vagina is designed to be self-cleaning but women may have a normal white or clear discharge.
- Hormonal changes during a woman’s menstrual cycle affect the amount and type of discharge her/their vagina produces.
- Unless a woman is having symptoms– such as pain during sex, itching, a foul-smelling discharge, or burning— her vagina needs little maintenance other than daily washing with mild soap and water.
- After a vaginal birth, the vagina may lose some of its elasticity and stretch more than usual but over time, most vaginas will return to almost prebirth size.
- Kegel exercises can help strengthen pelvic floor muscles and restore vaginal tone.
- The inner labia may darken due to hormonal changes after age 29. As estrogen levels in the body decrease, the vaginal walls become thinner and drier.
- Moisturizers or creams may help combat vaginal dryness and lubricants may help with intercourse [16].
- During menopause, the vulva may appear shrunken; vaginal atrophy is a common problem for many women.
- Atrophy may occur in the urethra and can lead to urine leakage, overactive bladder, and urinary incontinence [17].
- Low estrogen may change the acidity in the vagina and may increase the risk of infection due to bacterial overgrowth. It can also impact the urinary tract [16].
Although CFReSHC patient-partners stated they experienced vaginal dryness, it is unclear if this occurs more frequently amongst the CF female population or why [18].
I have gastroparesis as a result of CF and it has caused severe pelvic pain and weakening of pelvic floor muscles so I’ve been doing exercises to make my pelvic floor stronger. However, treatment for the gastroparesis lead to frequent UTI’s, which I was also treated for, but it was just another inconvenient bump in the road.

Peer to Peer Advice
- Your vagina is self-cleaning. Use unscented and pH balanced soaps and avoid douching, baby powder and perfumed lotions to maintain optimal vaginal health.
- Wearing cotton panties (no thongs) and avoiding tight clothes might help reduce yeast infections.
- Boric Acid suppository (not used during pregnancy) is an OTC remedy for bacterial vaginosis.
- Do not douche as it is not healthy.
- Avoid shaving/removing pubic hair. Pubic hair was put there to protect your genitalia from friction and infection
- Using cool packs may help with vaginal pain.
- Rinse the vulva with water after peeing to help lower pain and irritation.
- Pat the vulva dry instead of rubbing it dry. The skin of your vulva is ultra sensitive, and it’s easily irritated by products with artificial additives (as many fragrant soaps, body washes, and moisturizers contain).
- Switch to cotton or organic menstrual pads to lessen the chance of allergy and irritation and keep pH balance in the vagina.
- Probiotics help with vaginal health. Cranberry juice is also beneficial for supporting healthy bacteria and preventing yeast infections.
- Clotrimazole cream is an over-the-counter option for yeast issues.
- A little itchiness in the vaginal area is normal. Still, if the vulva/vagina becomes excessively itchy or has cheesy discharge, you might have a yeast infection, and it’s best to see a gynecologist and get treatment.
- When wiping the vaginal area, wipe from front to back to avoid spreading bacteria.
- Mental health and self-care are related. Try to ensure that both are addressed.
Results from the CFReSHC Snap Poll
A CFReSHC Snap poll (n=80) on the topic of vaginal health allowed respondents to identify and rank which research topics they found important:
- How does CFRD play a role in chronic yeast infections? (55.6%)
- How much do our cervical mucus issues play a role in our vaginal health? (54.2%)
- Do women with CF have more vaginal discharge? Different kinds of vaginal discharge? (50%)
At what age do we start to see vaginal changes in women with CF? (44.4%) [11].
Resource Links
Works Cited
- Kazmerski TM, Sawicki GS, Miller E, et al. Sexual and reproductive health behaviors and experiences reported by young women with cystic fibrosis. Journal of Cystic Fibrosis. 2018;17(1):57-63. http://dx.doi.org/10.1016/j.jcf.2017.07.017. doi: 10.1016/j.jcf.2017.07.017.
- Longo L, Speri A, Sartori G, Doro R. Preliminary results of a nurse-led study cystic fibrosis center of Veneto, Verona, Italy. Abstract. J Cystic Fibrosis. 2002;1:S81–S180.
- Rousset Jablonski C, Reynaud Q, Perceval M, et al. Contraceptive practices and cervical screening in women with cystic fibrosis. Human Reproduction. 2015;30(11):2547-2551. https://www.ncbi.nlm.nih.gov/pubmed/26345688. doi: 10.1093/humrep/dev217.
- Cystic Fibrosis Foundation. How does CF affect the female reproductive system. https://www.cff.org/Life-With-CF/Transitions/Reproductive-Health-and-Fertility/How-Does-CF-Affect-the-Female-Reproductive-System.
- Chambers R, Chambers R, Lucht A, et al. Prevalence and impact of pelvic floor dysfunction in an adult cystic fibrosis population: A questionnaire survey. Int Urogynecol J. 2017;28(4):591-604. https://www.ncbi.nlm.nih.gov/pubmed/27738735. doi: 10.1007/s00192-016-3152-z.
- Rousset Jablonski C, Reynaud Q, Perceval M, et al. Contraceptive practices and cervical screening in women with cystic fibrosis. Human Reproduction. 2015;30(11):2547-2551. https://www.ncbi.nlm.nih.gov/pubmed/26345688. doi: 10.1093/humrep/dev217.
- National Vulvodynia Association. The latest news, information and studies on vulvodynia. https://www.nva.org.
- Nelson A, De Soyza A, Perry JD, Sutcliffe IC, Cummings SP. Polymicrobial challenges to koch’s postulates: Ecological lessons from the bacterial vaginosis and cystic fibrosis microbiomes. Innate immunity (London, England). 2012;18(5):774-783. https://search.datacite.org/works/10.1177/1753425912439910. doi: 10.1177/1753425912439910.
- Baldwin S. CFReSHC patient task force presentation on vaginal health. 2.12.2020.
- Baldwin SB. CFReSHC patient task force presentation on vaginal health. 2.23.2019.
- Chin‐Hong PV. Time to take on HPV in the Transplant clinic — warts and all. American Journal of Transplantation. 2019;19(1):11-12. https://onlinelibrary.wiley.com/doi/abs/10.1111/ajt.15108. doi: 10.1111/ajt.15108.
- Cyganek A, Pietrzak B, Wielgoś M, Grzechocińska B. Menopause in women with chronic immunosuppressive treatment – how to help those patients. Przegla̜d menopauzalny. 2016;15(1):1-5. https://www.ncbi.nlm.nih.gov/pubmed/27095951. doi: 10.5114/pm.2016.58765.
- Sauerbrei A. Herpes genitalis: Diagnosis, treatment and prevention. Geburtshilfe und Frauenheilkunde. 2016;76(12):1310-1317. http://dx.doi.org/10.1055/s-0042-116494. doi: 10.1055/s-0042-116494.
- CF Reproductive and Sexual Health Collaborative. CFReSHC snap poll of vaginal health treatment options. 5.16.2020.
- Irving G, Miller D, Robinson A, Reynolds S, Copas AJ. Psychological factors associated with recurrent vaginal candidiasis: A preliminary study. Sexually Transmitted Infections. 1998;74(5):334-338. http://dx.doi.org/10.1136/sti.74.5.334. doi: 10.1136/sti.74.5.334.
- McDermott A. What you need to know about vaginal health at every age. Healthline. 2016.
- Johannesson M, Carlson M, Brucefors AB, Hjelte L. Cystic fibrosis through a female perspective: Psychosocial issues and information concerning puberty and motherhood. Patient Education and Counseling. 1998;34(2):115-123.
http://dx.doi.org/10.1016/S0738-3991(97)00087-6. doi: 10.1016/S0738-3991(97)00087-6.
- CF Reproductive and Sexual Health Collaborative. CFReSHC patient task force meeting on vaginal health. 2.12.2020.
Free Printable PDF Download
Want a free printable PDF download of this section for your use in clinic? Just give us your name and email address below to get your download link. This will not add you to our email list.